Wholistic Therapies
Autoimmune Diseases
Definition
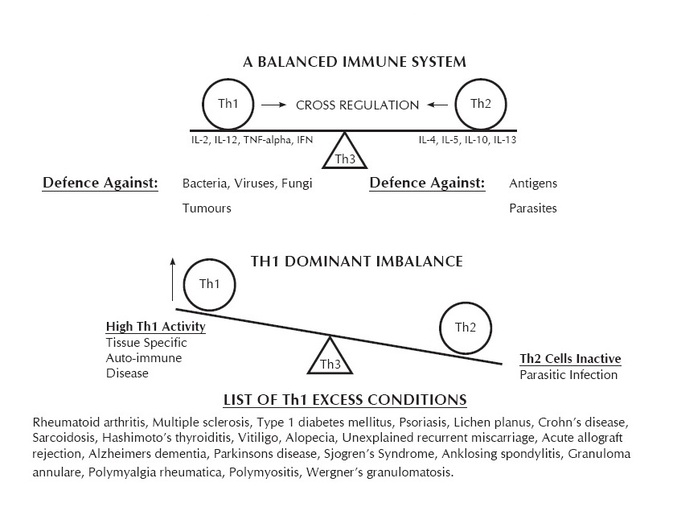
Autoimmunity is defined as an inappropriate reaction of the immune system to the body’s own tissues. It is characterised by a loss of discrimination of self from non-self tissues, and leads to an ongoing and often severe inflammatory response. This response is mediated via T-Helper cells, which direct the rest of the immune system’s actions. Two broad classes of T-Helper cells exist, with T-Helper 1 cells directing the cell-mediated immune response, and T-Helper 2 directing the antibody-mediated response.5 5 Feb10
Autoimmune diseases can be categorised based on the T-Helper cells that drive them. This is done largely by analysing the levels of characteristic cytokines present, which indicate the type of T-Helper cell activity. It is important to be aware however, that some conditions may present with both patterns, or with one in an early stage, followed by the other later. This makes analysis of conditions for inclusion in TH1 or TH2 tables very difficult. The lists provided represent our best current understanding of the research into these conditions.
See table on last page for a list of diseases that are associated with T-Helper 1 dominance.
Aetiology / Risk Factors
Despite extensive investigation, no consistent pattern regarding the cause of autoimmunity has emerged. Some possibilities include
• Genetic / inherited causes
• Infection with organisms that have a similar molecular signature to body tissues, leading to confusion of the immune system (molecular mimicry)
• Chemicals or infections that alter self-antigens
• Stress
Diet and Lifestyle
• Eliminate all food allergens from the diet. The most common allergenic foods are dairy, soy, citrus, peanuts, wheat, fish, eggs, corn, food colourings, and additives. An elimination/challenge trial may be helpful in uncovering sensitivities, or an IgG ELISA food allergy test may be used. Remove suspected allergens from the diet for at least two weeks. Re-introduce foods at the rate of one food every three days. Watch for reactions which may include gastrointestinal upset, mood changes, headaches, and exacerbation of asthma. Warning: Do not challenge peanuts, or any other food if there is history of anaphylaxis.
• Reduce pro-inflammatory foods in the diet including saturated fats (meats, especially poultry, and dairy), refined foods, and sugar. Patients sensitive to antibiotics should eat only organic meats to avoid antibiotic residues.
• A small percentage of people respond dramatically to a diet free of nightshades. They include peppers, eggplant, tomatoes, and white potatoes. A month-long trial is recommended.
• Emphasise foods high in essential fatty acids such as oily fish and nuts / seeds
• Eat a minimally processed diet rich in antioxidants, phytonutrients and bioflavonoids
• Protein is essential for connective tissue support and should be consumed regularly
• Nutrients to support digestive health including fibre and yoghurt should be consumed if tolerated to enhance beneficial bacterial levels
• Stress management techniques should be implemented
My recommendation for all autoimmune diseases including;
Rheumatoid Arthritis, Diabetis type 1, Psoriasis, Crohn's disease, Hashimoto's Thyroiditis, Vitiligo, Alopecia, Alzheimer's dementia, Parkinson's disease, Sjogren's Syndrome and Multiple Sclerosis, is the TH1 Balance containing, Polypodium Leucatomos and Vitamin D3.
Autoimmunity is defined as an inappropriate reaction of the immune system to the body’s own tissues. It is characterised by a loss of discrimination of self from non-self tissues, and leads to an ongoing and often severe inflammatory response. This response is mediated via T-Helper cells, which direct the rest of the immune system’s actions. Two broad classes of T-Helper cells exist, with T-Helper 1 cells directing the cell-mediated immune response, and T-Helper 2 directing the antibody-mediated response.5 5 Feb10
Autoimmune diseases can be categorised based on the T-Helper cells that drive them. This is done largely by analysing the levels of characteristic cytokines present, which indicate the type of T-Helper cell activity. It is important to be aware however, that some conditions may present with both patterns, or with one in an early stage, followed by the other later. This makes analysis of conditions for inclusion in TH1 or TH2 tables very difficult. The lists provided represent our best current understanding of the research into these conditions.
See table on last page for a list of diseases that are associated with T-Helper 1 dominance.
Aetiology / Risk Factors
Despite extensive investigation, no consistent pattern regarding the cause of autoimmunity has emerged. Some possibilities include
• Genetic / inherited causes
• Infection with organisms that have a similar molecular signature to body tissues, leading to confusion of the immune system (molecular mimicry)
• Chemicals or infections that alter self-antigens
• Stress
Diet and Lifestyle
• Eliminate all food allergens from the diet. The most common allergenic foods are dairy, soy, citrus, peanuts, wheat, fish, eggs, corn, food colourings, and additives. An elimination/challenge trial may be helpful in uncovering sensitivities, or an IgG ELISA food allergy test may be used. Remove suspected allergens from the diet for at least two weeks. Re-introduce foods at the rate of one food every three days. Watch for reactions which may include gastrointestinal upset, mood changes, headaches, and exacerbation of asthma. Warning: Do not challenge peanuts, or any other food if there is history of anaphylaxis.
• Reduce pro-inflammatory foods in the diet including saturated fats (meats, especially poultry, and dairy), refined foods, and sugar. Patients sensitive to antibiotics should eat only organic meats to avoid antibiotic residues.
• A small percentage of people respond dramatically to a diet free of nightshades. They include peppers, eggplant, tomatoes, and white potatoes. A month-long trial is recommended.
• Emphasise foods high in essential fatty acids such as oily fish and nuts / seeds
• Eat a minimally processed diet rich in antioxidants, phytonutrients and bioflavonoids
• Protein is essential for connective tissue support and should be consumed regularly
• Nutrients to support digestive health including fibre and yoghurt should be consumed if tolerated to enhance beneficial bacterial levels
• Stress management techniques should be implemented
My recommendation for all autoimmune diseases including;
Rheumatoid Arthritis, Diabetis type 1, Psoriasis, Crohn's disease, Hashimoto's Thyroiditis, Vitiligo, Alopecia, Alzheimer's dementia, Parkinson's disease, Sjogren's Syndrome and Multiple Sclerosis, is the TH1 Balance containing, Polypodium Leucatomos and Vitamin D3.
